Diabetes & Your Eyes
Dilated Eye Exams Can Detect Diabetes
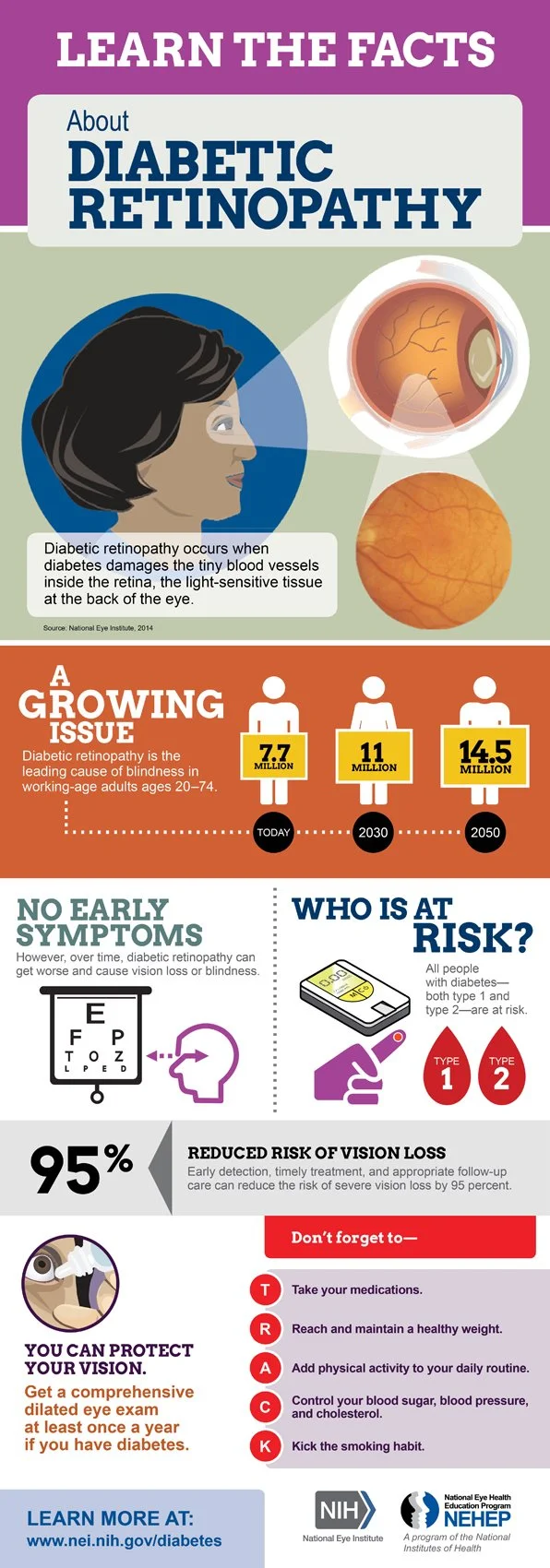
Diabetic Retinopathy
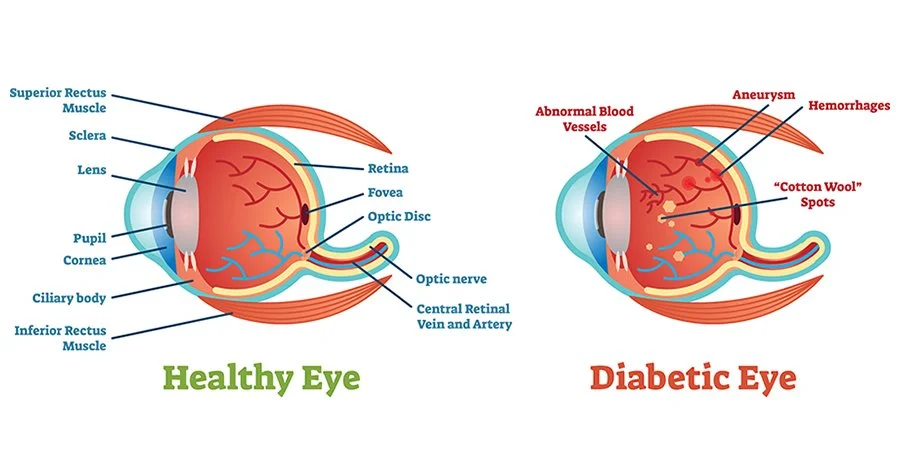
Diabetic retinopathy is a serious condition in which diabetes damages blood vessels in the rear of the eye, causing progressive damage to the retina, the light-sensitive lining at the back of the eye. Tiny blood vessels leak blood and other fluids. This causes the retinal tissue to swell, resulting in cloudy or blurred vision. Diabetic retinopathy usually affects both eyes. If left untreated, diabetic retinopathy can cause blindness. Fortunately, treatments are available that can reduce the chances that vision loss will progress.
When people with diabetes experience long periods of high blood sugar, fluid can accumulate in the lens inside the eye that controls focusing. This changes the curvature of the lens, leading to changes in vision. However, once blood sugar levels are controlled, usually the lens will return to its original shape and vision improves. Patients with diabetes who better control their blood sugar levels will slow the onset and progression of diabetic retinopathy. You can greatly reduce your risk of vision loss from diabetic retinopathy by managing your overall health and your diabetes.
Diabetic retinopathy damaged blood vessels can cause vision loss:
Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision.
In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision.
Non-proliferative diabetic retinopathy
NPDR is the early stage of the disease in which symptoms will be mild or nonexistent. In NPDR, the blood vessels in the retina are weakened. Tiny bulges in the blood vessels may leak fluid into the retina. This leakage may lead to swelling of the macula.
Proliferative diabetic retinopathy
Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease. At this stage, circulation problems deprive the retina of oxygen. As a result, new, fragile blood vessels can begin to grow in the retina and into the vitreous, the gel-like fluid that fills the back of the eye. The new blood vessels may leak blood into the vitreous, clouding vision.
Other complications of PDR include detachment of the retina due to scar tissue formation and the development of glaucoma. Glaucoma is an eye disease in which there is progressive damage to the optic nerve. In PDR, new blood vessels grow into the area of the eye that drains fluid from the eye. This greatly raises the eye pressure, which damages the optic nerve. If left untreated, PDR can cause severe vision loss and even blindness.
Risk factors for diabetic retinopathy include:
Diabetes. People with type 1 or type 2 diabetes are at risk for developing diabetic retinopathy. The longer a person has diabetes, the more likely he or she is to develop diabetic retinopathy, particularly if the diabetes is poorly controlled.
Race. Hispanics and African Americans are at greater risk of developing diabetic retinopathy.
Medical conditions. People with other medical conditions, such as high blood pressure and high cholesterol, are at greater risk.
Pregnancy. Pregnant women face a higher risk of developing diabetes and diabetic retinopathy. If a woman develops gestational diabetes, she has a higher risk of developing diabetes as she ages.
Family History.
Symptoms
Symptoms of diabetic retinopathy include:
Seeing spots or floaters.
Blurred vision.
Having a dark or empty spot in the center of your vision.
Difficulty seeing well at night.
Diagnosis
Diabetic retinopathy can be diagnosed through a comprehensive eye examination. Testing, with emphasis on evaluating the retina and macula, may include:
Patient history to determine vision difficulties, presence of diabetes, and other general health concerns that may be affecting vision.
Visual acuity measurements to determine how much central vision has been affected.
Refraction to determine if a new eyeglass prescription is needed.
Evaluation of the ocular structures, including the evaluation of the retina through a dilated pupil.
Measurement of the pressure within the eye.
Supplemental testing may include:
Retinal photography or tomography to document the current status of the retina.
Fluorescein angiography to evaluate abnormal blood vessel growth.
Treatment
Treatment of diabetic retinopathy varies depending on the extent of the disease. People with diabetic retinopathy may need laser surgery to seal leaking blood vessels or to discourage other blood vessels from leaking. A doctor of optometry might need to inject medications into the eye to decrease inflammation or stop the formation of new blood vessels. People with advanced cases of diabetic retinopathy might need surgical intervention.
If you are diabetic, you can help prevent or slow the development of diabetic retinopathy by:
Taking your prescribed medication.
Maintaining a healthy diet.
Exercising regularly.
Controlling high blood pressure.
Avoiding alcohol and smoking.
Prevention
Blood sugar control (glycemic control).
Blood Pressure Control—BP of less than 140/80 mm Hg for a patient with diabetes.
Lipid Lowering—lowering LDL cholesterol through lifestyle modification. Lowering saturated fats and cholesterol, weight loss, increase physical activity, use of statins for reducing high cholesterol.
Weight management—being overweight is associated with increased risk of Type 2 Diabetes.